Healthcare Softwares: Types, Use Cases, and How to Choose in 2026
Alexander Stasiak
Feb 03, 2026・10 min read
Table of Content
Top Types of Healthcare Software in 2026
Electronic Health Records (EHR) and Personal Health Records (PHR)
Practice Management and Hospital Information Systems (PMS/HIS)
Telemedicine and Virtual Care Platforms
Remote Patient Monitoring (RPM) and mHealth Apps
Clinical Decision Support Systems (CDSS) and Medical Knowledge Bases
Medical Imaging, PACS, and Diagnostic Software
Laboratory Information Management Systems (LIMS)
Medical Billing, Coding, and Revenue Cycle Management (RCM) Software
Pharmacy Management and E-Prescribing Software
Inventory, Asset, and Medical Equipment Management Software
Medical Research, Clinical Trial, and Data Analytics Platforms
Key Considerations When Choosing Healthcare Software
Define Clinical, Operational, and Patient Experience Priorities
Evaluate Usability, Training Needs, and Change Management
Assess Interoperability, Standards, and Integration Complexity
Prioritize Security, Privacy, and Regulatory Compliance
Balance Total Cost of Ownership with Long-Term Value
Security, Privacy, and Interoperability in Healthcare Softwares
Health Data Security and Common Cyber Threats
Compliance with HIPAA, GDPR, and Other Regulations
Interoperability and Semantic Consistency
Emerging Technologies Shaping Healthcare Softwares
Artificial Intelligence and Machine Learning in Clinical and Operational Workflows
Internet of Things (IoT) and Connected Medical Devices
Extended Reality (AR/VR) for Training, Therapy, and Surgery
Blockchain and Advanced Data Governance
Strategic Takeaways: Building a Future-Ready Healthcare Software Ecosystem
Build a Future-Ready Healthcare IT Stack
Get expert help choosing compliant, secure, interoperable healthcare software👇
The global healthcare IT market is projected to surpass $500 billion by 2030, driven by a fundamental shift in how care is delivered, documented, and coordinated. Since the COVID-19 pandemic accelerated digital adoption across hospitals and clinics worldwide, healthcare organizations have moved decisively away from paper-based workflows and disconnected systems toward integrated digital platforms. Modern healthcare now depends on electronic health records, telemedicine, analytics, and AI working together to reduce documentation burden, connect patient data across providers, and improve health outcomes. Whether you run a solo practice or manage IT for a 500-bed hospital, the software decisions you make today will define your organization’s ability to deliver efficient, safe, and patient-centered care.
This guide will walk you through the main types of healthcare software in use today, explain how to evaluate and choose the right solutions for your organization, and highlight where the market is heading through 2026 and beyond.
Top Types of Healthcare Software in 2026
This section provides a practical overview of the most widely used healthcare software categories in 2026, focusing on real-world applications across hospitals, outpatient clinics, and digital health startups. The list combines clinical, administrative, and patient-facing tools that together form a typical healthcare IT stack.
The exact mix of software your organization needs depends on its size—a solo practice has different requirements than a multi-hospital health system—and your regulatory environment. Organizations in the United States must comply with HIPAA, while those handling EU patient information must address GDPR requirements. The following subsections describe each software type, its main benefits, and typical buyers and users.
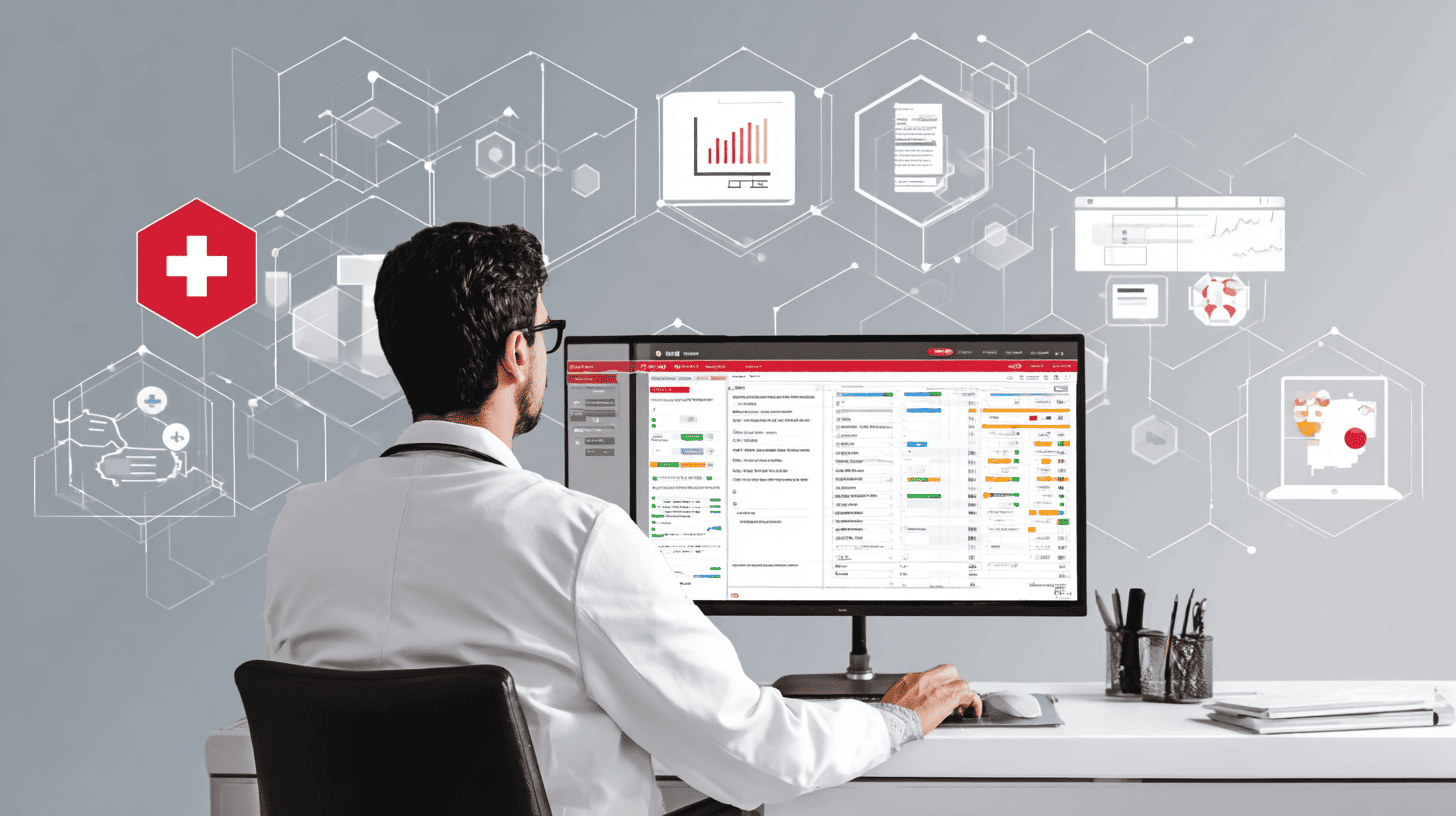
Electronic Health Records (EHR) and Personal Health Records (PHR)
Electronic Health Records represent the longitudinal, provider-managed digital record of a patient’s medical history, including diagnoses, medications, allergies, lab results, imaging reports, and procedures. Personal Health Records, by contrast, are patient-managed health information repositories, often accessed via mobile apps or patient portals that connect patients directly to their healthcare data.
Major EHR vendors like Epic Systems (deployed across more than 250 major US healthcare organizations managing records for 250 million patients), Oracle Health (formerly Cerner), and eClinicalWorks dominate the market. Adoption has been driven by meaningful use requirements in the United States and interoperability mandates built on standards like HL7 FHIR, which enables faster and more flexible data exchange compared to older protocols.
Key EHR capabilities include clinical charting, e-prescribing, computerized provider order entry (CPOE), lab and imaging integration, documentation templates, and embedded clinical decision support. Studies show that EHRs have reduced medication error rates by 55% in implementations with robust alert systems. PHR and patient portals extend these benefits by letting patients view lab results, request prescription refills, send secure messaging to clinicians, and download visit summaries—all of which improve patient engagement and treatment adherence.
It’s worth clarifying the differences between related terms. EMR (Electronic Medical Record) typically refers to a digital record maintained within a single provider’s practice and is often siloed. EHR emphasizes interoperability and the ability to share data securely across different healthcare facilities. PHR puts control in the patient’s hands, aggregating information from multiple sources into a single personal health data repository.
Practice Management and Hospital Information Systems (PMS/HIS)
Practice management software serves small to mid-sized clinics, while hospital information systems provide the comprehensive infrastructure needed for multi-department hospitals and large health systems. Both categories address the operational workflows that keep healthcare facilities running smoothly.
Core functions include appointment scheduling, patient registration, insurance eligibility verification, medical billing and claims processing, bed management for inpatient facilities, ward workflows, and discharge planning. Consider a 20-provider multispecialty clinic that implements a modern practice management system with automated appointment reminders and online booking. Such a clinic can realistically expect to cut no-show rates by 15% or more, recovering significant revenue that would otherwise be lost to empty appointment slots.
Hospital information systems scale these capabilities to manage the complexity of large facilities. They incorporate modules for laboratory management, pharmacy operations, financial analytics, and staff scheduling. Organizations that have integrated HMS platforms report operational cost reductions of 20-30% through automation of manual processes like payroll processing and claims management.
For these systems to deliver maximum value, tight integration with the EHR, radiology information systems, and billing platforms is essential. Without seamless data flow, staff end up entering the same information multiple times, increasing both workload and error rates.
Telemedicine and Virtual Care Platforms
Telemedicine platforms enable secure video, audio, and chat consultations between healthcare providers and patients, along with supporting functions like triage, scheduling, and e-prescribing. The surge of telehealth visits between 2020 and 2022 transformed virtual care from a convenience into a necessity, and continued reimbursement support in the United States and parts of Europe has sustained adoption.
Key platform features include HIPAA-compliant video conferencing, integrated payment processing, virtual waiting rooms, digital intake forms, and automatic documentation that flows directly into the EHR. Beyond synchronous video visits, virtual care now encompasses asynchronous messaging, remote triage chatbots, and specialist teleconsults that connect rural hospitals with urban medical centers.
A rural hospital without on-site cardiology coverage can now arrange teleconsults with specialists at academic medical centers, enabling timely intervention for patients who would otherwise face long drives or dangerous delays. Similarly, behavioral health follow-ups via telemedicine software have proven particularly effective, with patients often finding it easier to engage with mental health services from the privacy of their homes.
Remote Patient Monitoring (RPM) and mHealth Apps
Remote patient monitoring software works in conjunction with connected devices—Bluetooth blood pressure cuffs, continuous glucose monitors, wearable ECG patches, and smart scales—to stream health data from patients’ homes directly to clinical dashboards.
Specific use cases include chronic disease management for heart failure, COPD, and diabetes; post-operative monitoring to catch complications early; and elderly care programs that help seniors age safely at home. According to CMS data, remote patient monitoring has demonstrated a 38% reduction in hospital readmissions for chronic disease patients enrolled in well-designed programs.
Reimbursement has been a significant growth driver. Remote patient monitoring software gained billing codes in the late 2010s that were expanded through 2024-2025, making these programs financially viable for healthcare organizations of all sizes.
Consumer health tracking apps—covering sleep, menstrual cycles, mental health, and fitness—complement clinical RPM when integrated via APIs and FHIR standards. The key benefits are straightforward: fewer emergency department visits, earlier clinical interventions, and improved patient outcomes for chronic conditions. However, organizations must prepare for the challenge of data overload, implementing workflows that filter and prioritize alerts so clinicians can focus on patients who truly need attention.
Clinical Decision Support Systems (CDSS) and Medical Knowledge Bases
Clinical decision support systems are tools embedded within EHRs or accessible via web and mobile health applications that provide evidence-based recommendations, alerts, and risk scores during clinical workflows. They assist healthcare professionals in making informed decisions at the point of care.
Rule-based alerts represent the traditional CDSS approach: drug-drug interaction warnings, allergy alerts, and lab value notifications that fire when certain conditions are met. AI-driven models have expanded these capabilities to include predictive risk scoring for conditions like sepsis, readmission risk, and deterioration in hospitalized patients.
Medical knowledge bases like UpToDate provide evidence summaries that clinicians can reference during patient encounters, while drug information tools offer formulary data, dosing guidance, and interaction checking. These tools help standardize care and support clinical decisions across the organization.
Typical CDSS outputs include:
- Drug interaction and allergy alerts
- Evidence-based order sets for common conditions
- Clinical care pathways with guideline-based recommendations
- Risk scores for sepsis, falls, readmissions, and other outcomes
The challenge is alert fatigue. When systems generate too many low-value notifications, medical staff begin ignoring them—including the critical ones. Successful implementations require careful tuning of alert thresholds and customization to local clinical guidelines.
Medical Imaging, PACS, and Diagnostic Software
Picture Archiving and Communication Systems (PACS) and Vendor Neutral Archives (VNA) form the core infrastructure for storing, retrieving, and sharing imaging studies including X-rays, CT scans, MRIs, PET scans, and ultrasounds. These systems have replaced film-based workflows across most healthcare facilities worldwide.
Dedicated imaging software enables radiologists to manipulate images, create 3D reconstructions, measure anatomical structures, and support image-guided procedures. The DICOM standard governs image data exchange, ensuring that imaging equipment from different manufacturers can communicate with archiving and viewing systems across institutions.
Since 2023, AI-powered imaging analysis has moved from research into clinical production. FDA-cleared algorithms now assist with automated detection of lung nodules, diabetic retinopathy screening, and stroke triage—identifying large vessel occlusions and routing patients to appropriate care faster than traditional workflows allow.
High image volumes demand robust infrastructure, both for real-time performance during diagnostic workups and for long-term archival policies that meet regulatory retention requirements while managing storage costs.
Laboratory Information Management Systems (LIMS)
Laboratory Information Management Systems serve as the digital backbone of clinical and diagnostic labs, handling sample accessioning, test ordering, result entry, quality control, and reporting. These systems track specimens from the moment blood is drawn through analysis and final result verification.
Modern lab workflows depend on barcoded specimen tracking. A blood sample receives a barcode at phlebotomy, maintains its identity through processing and analysis, and has its results automatically verified and transmitted to the ordering provider’s EHR. This continuous monitoring eliminates the handwriting errors and specimen mix-ups that plagued paper-based labs.
Regulatory requirements shape LIMS functionality significantly. Systems must maintain detailed audit trails, support CLIA and ISO 15189 compliance, and facilitate external proficiency testing. Benefits include reduced turnaround time, fewer specimen identification errors, and automated reporting to public health registries for reportable conditions.
The high-throughput COVID-19 and respiratory virus testing demands of 2020-2023 accelerated LIMS investments across the industry, with many labs upgrading to cloud-based platforms capable of handling surge capacity.
Medical Billing, Coding, and Revenue Cycle Management (RCM) Software
Revenue cycle management software manages the financial life cycle of a patient encounter from insurance verification through claim submission to payment posting. These tools are essential for maintaining the financial performance of any healthcare organization.
Modern RCM platforms support ICD-10, CPT/HCPCS, and local coding schemes, providing automated claim scrubbing to catch errors before submission, denial management workflows, and financial analytics dashboards. Integration with EHR and practice management systems allows clinical documentation to feed coding and billing with minimal manual intervention.
Consider a mid-size orthopedic group struggling with high days in accounts receivable. By implementing automated pre-authorization workflows and clean claims scrubbing, the practice can identify and correct billing errors before submission, reduce denial rates, and accelerate collections. Organizations with mature RCM processes routinely achieve clean claim rates above 95%, translating directly to improved cash flow and cost reduction.
For healthcare administrators and finance leaders, the key evaluation criteria include denial analytics, automated eligibility verification, and integration depth with clinical systems. The goal is minimizing the administrative tasks that consume staff time without generating revenue.
Pharmacy Management and E-Prescribing Software
Pharmacy management systems support both hospital and retail pharmacy operations: inventory control, dispensing workflows, compounding management, and controlled substance monitoring. These systems ensure that the right medication reaches the right patient in the right dose.
E-prescribing software enables clinicians to send prescriptions electronically to pharmacies, check formulary coverage, and receive refill requests—all within the clinical workflow. National e-prescribing mandates in the United States, along with electronic prior authorization requirements, have driven near-universal adoption among healthcare providers.
Safety benefits are substantial. E-prescribing systems perform allergy checking, pediatric dose range verification, and real-time drug interaction alerts at the point of prescribing. Networks like Surescripts, which processes approximately 80% of US e-prescriptions, have reduced prescription errors by 66% compared to handwritten or phoned prescriptions.
Inventory, Asset, and Medical Equipment Management Software
These tools track both consumables (syringes, PPE, implants, medical supplies) and capital assets (ventilators, infusion pumps, imaging devices) across healthcare facilities. Effective inventory management directly impacts both patient safety and financial operations.
Modern systems use barcodes and RFID tags integrated with purchasing platforms to trigger automatic reordering and prevent stockouts. Consider orthopedic or cardiac procedures involving implants: tracking software maintains a complete chain of custody for each implant, enabling rapid response if a manufacturer issues a recall and supporting accurate cost accounting per procedure.
Maintenance scheduling capabilities ensure that medical devices are calibrated and compliant with regulatory requirements, reducing downtime and safety risks. During supply chain disruptions like those experienced in 2020-2021, organizations with mature inventory systems were better positioned to identify shortages early and source alternatives.
Medical Research, Clinical Trial, and Data Analytics Platforms
Research platforms encompass clinical trial management systems (CTMS), electronic data capture (EDC) tools, and research databases like REDCap that support prospective studies. These systems help research teams design protocols, manage subject enrollment, track adverse events, and generate regulatory-compliant datasets for analysis and submission.
Healthcare analytics platforms combine clinical, operational, and financial data to produce dashboards tracking metrics like readmission rates, length of stay, cost per case, and population health outcomes. Since approximately 2022, cloud-based, AI-enabled analytics platforms have increasingly leveraged real-world data from EHRs and claims databases for outcomes research and medical research applications.
The connection between research and clinical care is tightening. Insights from analytics platforms feed back into clinical workflows, supporting data driven decisions at the bedside. A health system might use predictive analytics to identify patients at high risk for readmission, triggering care coordination interventions before discharge.
Key Considerations When Choosing Healthcare Software
Software buying decisions should not be driven solely by feature checklists. The right system for your organization depends on fit with existing clinical workflows, regulatory requirements, and long-term strategic direction. Poorly chosen systems increase clinician burnout and operational costs, while well-selected platforms free medical professionals to focus on patient care rather than fighting their tools.
The following subsections provide practical evaluation steps that a CIO, CMIO, or practice owner can follow when selecting healthcare solutions.
Define Clinical, Operational, and Patient Experience Priorities
Start with structured discovery sessions involving clinicians, nurses, medical staff, billing personnel, and patients to identify your top 5-7 pain points. These might include slow documentation, high claim denial rates, appointment scheduling bottlenecks, or difficulty accessing patient records across locations.
Map each pain point to specific software capabilities. Slow documentation might require templated notes and voice-to-text integration. High denials might call for integrated claims scrubbing and automated eligibility verification. Scheduling problems might need online booking, automated reminders, and waitlist management.
A primary care clinic’s priorities likely differ from a surgical center’s. The clinic might prioritize chronic disease registries, patient portal engagement, and care gap identification. The surgical center needs robust OR scheduling, implant tracking, and resource allocation tools. Understanding these differences prevents purchasing software optimized for the wrong use case.
Before implementation, measure baseline KPIs: no-show rates, claim denial percentages, documentation time per encounter, and patient satisfaction scores. These metrics provide the foundation for demonstrating ROI after the new system goes live.
Evaluate Usability, Training Needs, and Change Management
Usability directly affects clinician burnout. Healthcare professionals consistently cite “click burden”—the number of clicks required to complete routine tasks—as a source of frustration with their software tools. Intuitive interfaces that minimize unnecessary steps are essential for adoption and satisfaction.
Effective evaluation requires hands-on demos with frontline users, not just IT staff. Consider usability scoring methods during demos and plan short pilot rollouts in one or two departments before enterprise-wide deployment. This approach surfaces workflow issues before they affect the entire organization.
Role-based training plans are essential. Identify super-users in each department who receive advanced training and can support colleagues. Plan for on-site or remote vendor support during the first 90 days after go-live, when questions and issues peak.
Watch for these usability red flags during evaluation:
- More than three clicks to complete common tasks
- Inability to customize views and workflows for different roles
- Poor mobile access or lack of offline capability
- Missing accessibility features (adjustable fonts, color contrast options)
- Cluttered screens with irrelevant information
Assess Interoperability, Standards, and Integration Complexity
Interoperability means the ability to exchange data effectively with existing systems—your EHR, lab information system, imaging archive, pharmacy system, and health information exchanges. A system that cannot communicate with your current technology stack will create data silos and duplicate work.
Understanding key standards helps frame vendor conversations. HL7 v2 is the legacy messaging standard still widely used for lab results and ADT messages. HL7 FHIR represents the modern approach, using web APIs for faster, more flexible integration. DICOM governs medical imaging exchange. Terminology standards like SNOMED CT, LOINC, and ICD-10 ensure that clinical concepts are coded consistently across systems.
Consider the difference between a fragmented workflow where lab results arrive by fax, requiring manual entry into the EHR, versus an integrated system where results post automatically with appropriate clinical alerts. The integrated approach saves time, reduces errors, and enables timely clinical response.
When evaluating vendors, ask about open APIs, published integration guides, and willingness to collaborate with third-party systems. Vendors who lock healthcare data behind proprietary formats create long-term strategic risk for your organization.
Prioritize Security, Privacy, and Regulatory Compliance
Healthcare software must comply with applicable regulatory frameworks. In the United States, HIPAA establishes requirements for privacy, security, and breach notification. The EU’s GDPR governs processing of EU residents’ personal data, requiring lawful basis, data minimization, and respect for individual rights. Canada’s PIPEDA and various local health data acts add additional requirements depending on your geography.
Concrete security features to evaluate include:
- Encryption in transit (TLS) and at rest
- Multi-factor authentication for all users
- Role-based access control limiting data visibility by job function
- Detailed audit logs tracking who accessed what and when
- Regular penetration testing and vulnerability assessments
During vendor selection, ask about incident response procedures, backup and restore testing frequency, and ransomware preparedness. Healthcare organizations are prime targets for ransomware attacks, and your vendors must demonstrate readiness to protect patient information.
For cloud services, ensure that vendors will sign Business Associate Agreements (BAAs) under HIPAA or equivalent data processing agreements under GDPR. Conduct due diligence on data residency—where patient data will be stored—and the vendor’s use of subcontractors.
Balance Total Cost of Ownership with Long-Term Value
Look beyond the license or subscription price to understand total cost of ownership over 5+ years. Factor in implementation services, data migration, training, integration development, and ongoing support costs. A system with a lower sticker price may prove more expensive when all costs are considered.
Pricing models vary by market segment. Small practices typically pay per-provider subscription fees. Large health systems negotiate enterprise licenses. Telemedicine software and analytics tools increasingly use usage-based pricing tied to visit volumes or data processed.
Consider a simple ROI approach: If a new system saves each clinician 30 minutes per day on documentation, that translates to 2.5 hours per week per provider. For a 10-provider practice, that’s 25 hours of recovered clinical capacity weekly—time that can be redirected to additional patient visits or reduced overtime costs. If the practice averages $150 per visit, even a modest increase in daily patient volume generates significant financial impact.
Vendor stability matters for long-term value. Evaluate the vendor’s financial health, product roadmap transparency, and history of delivering promised upgrades. A vendor that stagnates or gets acquired may leave you with a dead-end system requiring costly replacement.
Security, Privacy, and Interoperability in Healthcare Softwares
Security, privacy, and interoperability form the non-negotiable foundation of any healthcare software deployment in 2026. Recent years have seen a dramatic rise in cyberattacks targeting healthcare organizations, with data breaches and ransomware incidents disrupting hospital operations and exposing sensitive data on millions of patients.
The following subsections address cyber threats, data protection practices, and the interoperability challenges that healthcare organizations must navigate.
Health Data Security and Common Cyber Threats
Healthcare organizations face a range of cyber threats. Phishing attacks trick staff into revealing credentials or clicking malicious links. Ransomware encrypts systems and demands payment for restoration, sometimes forcing hospitals to divert patients and cancel surgeries. Insider threats—whether malicious or accidental—expose patient data through unauthorized access or careless data handling. Even medical devices like infusion pumps can be compromised, with potentially life-threatening consequences.
Healthcare data breaches have reached alarming scale. In 2021 alone, breaches affected 116 million patient records in the United States. The impact extends beyond regulatory fines: hospitals have faced appointment cancellations, EHR downtime lasting days or weeks, and lasting reputational damage.
Medical records are more valuable than credit card data on black markets because they contain information useful for identity theft, insurance fraud, and other crimes that can go undetected for years. This makes healthcare facilities particularly attractive targets.
Layered defenses are essential. Network segmentation limits lateral movement if attackers breach one system. Rigorous patch management closes known vulnerabilities. Endpoint protection detects and blocks malware. Staff training reduces phishing success rates. Zero-trust principles—verifying every access request regardless of source—add another layer of protection.
Compliance with HIPAA, GDPR, and Other Regulations
HIPAA’s core rules establish the regulatory baseline for US healthcare organizations. The Privacy Rule governs how protected health information can be used and disclosed. The Security Rule requires administrative, physical, and technical safeguards for electronic health data. The Breach Notification Rule mandates reporting of breaches to affected individuals, HHS, and in some cases the media.
GDPR applies to any organization processing personal data of EU residents. Key obligations include establishing a lawful basis for processing, practicing data minimization, managing consent appropriately, and honoring individuals’ rights to access, correct, and delete their data where applicable.
For organizations operating across borders or in other jurisdictions, additional regulations apply—PIPEDA in Canada, Australia’s Privacy Act, and various national health data laws require attention.
Cloud providers handling healthcare data must sign Business Associate Agreements (BAAs) under HIPAA or equivalent data processing agreements under GDPR. Conduct due diligence on where data will be stored and whether the vendor uses subcontractors who also handle sensitive data. Regulatory compliance is a shared responsibility between your organization and your vendors.
Interoperability and Semantic Consistency
Technical interoperability—the ability to send and receive data—is necessary but not sufficient. Semantic interoperability ensures that receiving systems interpret data the same way the sending system intended. A lab result code that means “glucose” in one system must mean the same thing in every other system that receives it.
Key standards enable this consistency:
- HL7 v2: Legacy messaging standard for lab results, admissions, and orders
- HL7 FHIR: Modern API-based standard enabling web-style data exchange
- DICOM: Standard for medical imaging data exchange
- CDA: Clinical Document Architecture for structured clinical documents
- SNOMED CT: Comprehensive clinical terminology for diagnoses and procedures
- LOINC: Standard codes for laboratory and clinical observations
Consider a patient who moves between two hospitals using different EHR systems. If both systems use standardized lab codes, the receiving hospital can immediately interpret the patient’s previous results. Without standardization, clinicians might repeat tests unnecessarily or misinterpret results, creating both cost and patient safety issues.
Regulators increasingly push for open data exchange through initiatives like the US 21st Century Cures Act and its information blocking rules. When evaluating vendors, ask for conformance statements documenting their implementation of key standards and proof of successful interoperability with other systems in your healthcare ecosystem.
Emerging Technologies Shaping Healthcare Softwares
Beyond core systems, emerging technologies like AI, IoT, and extended reality are reshaping how care is delivered and coordinated. These are no longer purely experimental. Since approximately 2022, many hospitals and health plans have launched pilot projects or scaled solutions incorporating cutting edge technology into clinical and operational workflows.
The following subsections outline practical applications and constraints rather than hype.
Artificial Intelligence and Machine Learning in Clinical and Operational Workflows
AI applications in healthcare have moved from research prototypes to production systems. Concrete use cases include image analysis for radiology (detecting lung nodules, identifying stroke findings), natural language processing for clinical note summarization, and predictive models for readmission risk and sepsis detection.
From 2023 through 2025, many health systems began piloting generative AI tools to draft visit summaries, prior authorization forms, and patient communication letters. These tools augment clinical workflows, with healthcare practitioners reviewing and editing AI-generated outputs rather than creating documents from scratch.
Challenges remain significant. AI models are only as good as their training data—biased datasets produce biased predictions. Explainability requirements demand that clinicians understand why an algorithm made a particular recommendation. Regulatory clearance is required when AI directly influences clinical decision making.
Human-in-the-loop oversight represents the current best practice. Machine learning tools can surface insights and draft content, but clinicians retain final responsibility for treatment plans and patient care decisions.
Internet of Things (IoT) and Connected Medical Devices
Healthcare IoT encompasses networks of connected devices feeding data into central platforms: smart infusion pumps, bedside telemetry monitors, wearable health trackers, and home monitoring equipment. These devices enable continuous monitoring that was previously impossible outside hospital walls.
Consider a heart failure program using connected scales and blood pressure cuffs to detect fluid overload before it becomes a crisis. Patients weigh themselves each morning at home; weight gains exceeding threshold values trigger alerts to care coordinators who can intervene with medication adjustments before the patient requires emergency care.
Challenges include connectivity reliability (especially for home-based devices), managing device fleets at scale, integrating data streams into EHRs, and cybersecurity for edge devices. A compromised infusion pump could theoretically deliver incorrect doses, making device security a patient safety priority.
Regulations increasingly treat connected health tools as medical devices, requiring manufacturers to meet safety and adverse event reporting requirements. Organizations deploying IoT solutions must understand which devices fall under medical device regulations and ensure appropriate compliance.
Extended Reality (AR/VR) for Training, Therapy, and Surgery
Augmented and virtual reality applications have found practical niches in healthcare delivery and education. Surgical planning platforms use 3D reconstructions to help surgeons visualize complex anatomy before entering the operating room. Medical students learn anatomy through immersive VR environments. Physical therapists use VR games to make rehabilitation exercises more engaging.
VR exposure therapy for PTSD and phobias has shown promising results, allowing patients to confront anxiety triggers in controlled virtual environments. AR overlays in orthopedic surgery help surgeons position implants with greater precision, overlaying planned placement on the surgical field.
Barriers to broader adoption include hardware costs, motion sickness in some users, the need for specialized content development, and evidence requirements from payers and regulators before coverage decisions. While not yet as ubiquitous as EHRs, AR/VR adoption has accelerated since 2020 with increasing clinical studies and pilot implementations.
Blockchain and Advanced Data Governance
Blockchain technology offers a distributed ledger approach for creating tamper-evident records, tracking consent, and documenting the provenance of clinical data as it moves across organizations.
Pilot concepts have explored portable patient health identities that travel with individuals across healthcare systems, tracking of high-value drug supply chains to prevent counterfeiting, and immutable audit trails for research datasets supporting regulatory submissions.
As of mid-2025, most blockchain healthcare projects remain in pilot or niche production stages rather than mainstream deployment. Scalability limitations, regulatory uncertainty, and interoperability with existing systems present ongoing challenges.
The realistic perspective: blockchain may eventually enable trusted data exchange across multiple organizations that lack established trust relationships, but it is not a cure-all for healthcare’s data challenges. Organizations should watch developments but avoid overcommitting to immature solutions.
Strategic Takeaways: Building a Future-Ready Healthcare Software Ecosystem
Healthcare software in 2026 spans a remarkable range—from foundational EHR and hospital management software to emerging AI and IoT applications. Interoperability and security form the essential infrastructure enabling all these systems to work together safely. The rise of connected devices and intelligent algorithms is creating new possibilities for virtual consultations, predictive care, and personalized treatment plans.
Key strategic recommendations for executives and clinical leaders:
- Think platforms, not point solutions. Isolated tools create data silos. Prioritize solutions that integrate with your existing systems and support seamless access to patient information across care settings.
- Invest in interoperability from the start. Systems built on open standards like FHIR and HL7 will adapt more easily as the healthcare ecosystem evolves. Ask vendors for proof of standards conformance.
- Involve clinicians early and often. The best software decisions emerge from structured input by the people who will use these tools daily. Discovery sessions, pilot testing, and ongoing feedback loops reduce implementation failures.
- Measure ROI systematically. Establish baseline metrics before implementation and track improvements in operational efficiency, revenue management, and improved patient outcomes after go-live.
- Plan for continuous evolution. Technology and regulations change constantly. Budget for ongoing training, upgrades, and periodic reassessment of your software portfolio every 2-3 years.
Healthcare software is not a one-time purchase but a continuous transformation journey. The organizations that streamline operations, connect patients to their care teams, and leverage data driven decisions will outperform those clinging to fragmented, outdated systems.
By 2030, healthcare delivery will be increasingly virtual, data-driven, and personalized. The software decisions you make today—prioritizing interoperability, security, usability, and strategic fit—will determine whether your organization leads that transformation or struggles to catch up.
Digital Transformation Strategy for Siemens Finance
Cloud-based platform for Siemens Financial Services in Poland

You may also like...

Mental health app features
Mental health apps have evolved far beyond meditation timers. In 2026, users expect personalized support, evidence-based content, strong safety features, and privacy-by-design.
Alexander Stasiak
Nov 30, 2025・10 min read
Understanding Custom Healthtech Software Development: A Clear Guide
When generic medical software slows you down, custom healthtech development can be the solution. Learn how tailored tools fit your unique workflow, improve patient care, and future-proof your healthcare operations.
Alexander Stasiak
Oct 08, 2025・8 min read
How AI Healthtech Companies Are Changing the Way We Look at Healthcare
AI healthtech companies are redefining how we experience healthcare. From accurate diagnoses to personalized treatments and streamlined hospital operations.
Alexander Stasiak
Oct 23, 2025・12 min read
Let’s build your next digital product — faster, safer, smarter.
Book a free consultationWork with a team trusted by top-tier companies.